If you haven't joined in a tweet chat before it's very simple. Here's a guide Tweet
Chat Details
Hosted by WeEOLC using #WeEOLC
This chat is guest hosted by @SarahFreer2
Introduction:
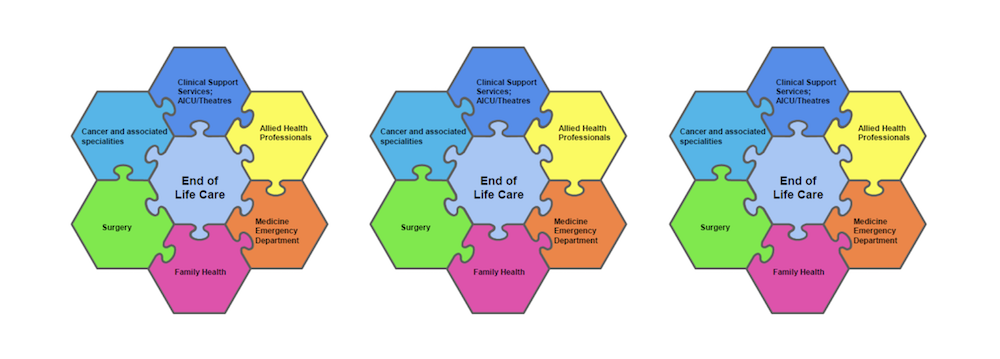
Developing and improving practice in End Of Life Care (EOLC) within a large NHS acute trust;
How do you engage a large workforce & drive up quality in EOLC when faced with increased and competing clinical service priorities?
This chat will focus on the role of the EOLC Champion as a means of sharing & developing initiatives around EOLC in the acute hospital.
National context:
Over the last few years there has been a national focus on improving the quality of end of life and the choices offered to patients and families across all settings. There has been many publications to guide;
- •National Palliative and End of life Partnership (2015) Ambitions for Palliative and End of Life care. A national framework 2015 - 2020•
- The Choice in End of life care programme (2015) What’s important to me;
- A review of choice in End of life care, Department of Health•
- CQC (2016) A different ending; Addressing inequalities in End of Life care Taking forward these new standards to enhance care is the challenge our trust has been tackling over the last 18 months.
Local Context:
It was recognised that as a trust we have national EOLC guidelines to achieve, whilst at the same time, there are local priorities that staff identified to improve practice in EOLC in their areas; both at a divisional level or at a more specialty level.
Introducing the EOLC Champion:
In September 2016, we embarked on introducing the role of the EOLC Champion across the trust. With the support of the Divisional Nurses across the 5 clinical divisions & specialities, nurses both registered & non registered, alongside allied health professionals have been identified as EOLC champions; staff who have an interest in EOLC, who can influence developments in EOLC that are pertinent to their clinical areas, & can further help to raise awareness and educate staff on key EOLC topics.
The champions are provided with quarterly trust wide meetings led by the hospital palliative care team. Alongside this, each division has 2 palliative care nurse specialists from the Hospital palliative care team linked to them, to support & facilitate developments, with the lead nurse for EOLC overseeing & feeding into the trust EOLC Steering group.
Benefits of EOL champion role:
- role model best practice
- act as a local resource for staff, patients and families
- identify areas for development to improve practice & be supported to achieve this development•cascade training to team members
- audit / benchmark palliative and end of life care
- share best evidence-based practice to sustain and embed change in the clinical area
There are now evolving developments:
- Critical care; EOLC champion structure across critical care, reviewing the care of those patients identified as EOL & who are transferred to a base ward; What needs improving? Developing relationships with the hospital palliative care team, looking towards discharging home for EOLC
- ED; Improvement to the relatives room, review of current use of the ‘viewing room’, improve the quality of EOLC for patients in the department – ensure they have a hospital bed, remove monitoring, commence end of life care plans provide info for relatives such as advice on car parking, providing refreshments, contacting the chaplains, how to contact the hospital etc.
- Allied Health professionals; local education on EOLC & their role, development of an information leaflet for families of patients at end of life: “Eating For Comfort” – eating and drinking at end of life, review of how we offer food to families of EOCL patients when in the hospital
So the question is - how are you facilitating developments in EOLC practice in your organisation?’
Chat Contributers
 100 Tweets
100 Tweets
200 Tweets
20000 Impressions
20000 Impressions
20000 Impressions
Engagement Wheel
Chat Word Cloud
Participant bio cloud
Chat Summary
Post Chat Comments
You'll need to be logged into via Twitter from the main menu, then you can share your post chat comments...
|
@{{Comment.screenName}}
{{Comment.DateCreated | date:"dd MMMM yyyy HH:mm"}}
|
{{Comment.Comment}} |
#WeEOLC transcript
|
@heblau
05 September 2017 20:00
|
Good evening, humans. Looking forward to tonight's chat on end of life care in acute hospitals. Subject very close to my heart #WeEOLC | |
|
@NUHEOLC
05 September 2017 20:00
|
RT @LesleyReilly20: #WeEoLC ready to go | |
|
@WeEOLC
05 September 2017 20:01
|
Let's all say "hello" and who you are With #WeEOLC in all tweets so we can see your thoughts! https://t.co/OUQLCnPbWF | |
|
@PhilBallRN
05 September 2017 20:02
|
Evening all, looking forward to this #WeEolc helping develop services across providers @vannapoulter @SarahVThompson @stowe_emily @WeEOLC | |
|
@LearnPEOLC
05 September 2017 20:02
|
Sarah here! #WeEOLC https://twitter.com/weeolc/status/905143926058876928 | |
|
@SarahFreer2
05 September 2017 20:02
|
#WeEOLC hello! ?? | |
|
@LesleyReilly20
05 September 2017 20:02
|
@WeEOLC #WeEOLC hello from lesley reilly division nurse NUH | |
|
@LearnPEOLC
05 September 2017 20:02
|
RT @WeEOLC: Let's all say "hello" and who you are With #WeEOLC in all tweets so we can see your thoughts! https://t.co/OUQLCnPbWF | |
|
@BridgetJohnst
05 September 2017 20:03
|
I'm here - Bridget, Glasgow and co facilitator of @WeEOLC #weeolc https://twitter.com/weeolc/status/905143926058876928 | |
|
@LearnPEOLC
05 September 2017 20:03
|
RT @hospicemanager: Evening all, looking forward to this #WeEolc helping develop services across providers @vannapoulter @SarahVThompson @s… | |
|
@JoyWharton1
05 September 2017 20:03
|
#WeEOLC Hi Joy here joining from Cumbria ???????? https://twitter.com/weeolc/status/905143524122927109 | |
|
@LeaBasra
05 September 2017 20:03
|
@WeEOLC Hello i currently work in a hosice interesting to learn how eolc works in a hospital #WeEOLC | |
|
@Nursey1982
05 September 2017 20:03
|
@WeEOLC Hello!! Sadie representing @teamEDnuh for tonight's #WeEOLC live chat! | |
|
@PhilBallRN
05 September 2017 20:03
|
RT @WeEOLC: Let's all say "hello" and who you are With #WeEOLC in all tweets so we can see your thoughts! https://t.co/OUQLCnPbWF | |
|
@NUHNursing
05 September 2017 20:03
|
@NUHNursing here #weeolc | |
|
@NUHNursing
05 September 2017 20:03
|
RT @BridgetJohnst: I'm here - Bridget, Glasgow and co facilitator of @WeEOLC #weeolc https://twitter.com/weeolc/status/905143926058876928 | |
|
@AgencyNurse
05 September 2017 20:04
|
Hello #weeolc listening in tonight - bad wifi so please forgive me if I am a bit behind | |
|
@WeEOLC
05 September 2017 20:04
|
hello Philip hanks for joining us! #WeEOLC @SarahFreer2 @NUHEOLC https://twitter.com/hospicemanager/status/905144062574985217 | |
|
@daljitathwal
05 September 2017 20:04
|
Hi Im @daljitathwal and here with the lovely @SarahFreer2 and team @NUHEOLC #WeEOLC https://twitter.com/WeEOLC/status/905143926058876928 | |
|
@StLukesPlymouth
05 September 2017 20:04
|
RT @WeEOLC: Not long to go until tonight's tweet chat with @SarahFreer2 @NUHEOLC http://www.wecommunities.org/tweet-chats/chat-details/2938 #WeEOLC https://t.co/lx5h1PuXlU | |
|
@NUHEOLC
05 September 2017 20:04
|
RT @Nursey1982: @WeEOLC Hello!! Sadie representing @teamEDnuh for tonight's #WeEOLC live chat! | |
|
@fionaDmurphy
05 September 2017 20:04
|
Hello #WeEoLC every patient and family every time = everyone's business ?? | |
|
@NUHEOLC
05 September 2017 20:04
|
RT @LeaBasra: @WeEOLC Hello i currently work in a hosice interesting to learn how eolc works in a hospital #WeEOLC | |
|
@suechisholm01
05 September 2017 20:04
|
@WeEOLC Hello, Sue Lead Cancer nurse at nuh ??#WeEOLC | |
|
@NUHEOLC
05 September 2017 20:04
|
RT @JoyWharton1: #WeEOLC Hi Joy here joining from Cumbria ???????? https://twitter.com/weeolc/status/905143524122927109 | |
|
@NUHEOLC
05 September 2017 20:06
|
RT @ruth_pettit: @WeEOLC #WeEOLC Hello from @ruth_pettit ?? I'm lead nurse for EOLC @NUHCriticalCare, we have about 15 champions for 58 cr… | |
|
@WeEOLC
05 September 2017 20:07
|
RT @LesleyReilly20: @WeEOLC #WeEOLC hello from lesley reilly division nurse NUH | |
|
@WeEOLC
05 September 2017 20:07
|
RT @SarahFreer2: #WeEOLC hello! ?? | |
|
@WeEOLC
05 September 2017 20:07
|
RT @learnhospice: Sarah here! #WeEOLC https://twitter.com/weeolc/status/905143926058876928 | |
|
@WeEOLC
05 September 2017 20:07
|
RT @hospicemanager: Evening all, looking forward to this #WeEolc helping develop services across providers @vannapoulter @SarahVThompson @s… | |
|
@WeEOLC
05 September 2017 20:08
|
RT @WeEOLC: Ok let's get straight into it! #WeEOLC Q1: how to support staff to engage in EOLC developments? @SarahFreer2… | |
|
@NUHNursing
05 September 2017 20:09
|
RT @SarahFreer2: #weEOLC & we re v proud of what you ve achieved! https://twitter.com/ruth_pettit/status/905144916052934657 | |
|
@AgencyNurse
05 September 2017 20:09
|
RT @WeEOLC: Ok let's get straight into it! #WeEOLC Q1: how to support staff to engage in EOLC developments? @SarahFreer2… | |
|
@WeNurses
05 September 2017 20:09
|
RT @WeEOLC: Ok let's get straight into it! #WeEOLC Q1: how to support staff to engage in EOLC developments? @SarahFreer2… | |
|
@vannapoulter
05 September 2017 20:09
|
What is everyone experience of end of life champions on general wards in general hospitals .... #WeEOLC | |
|
@WeEOLC
05 September 2017 20:09
|
#WeEOLC lots and lots of experience tonight - dont forget to add #WeEOLC to all your tweets and I'll be posting questions througout the chat | |
|
@NurseJoe87
05 September 2017 20:09
|
@WeEOLC @SarahFreer2 @NUHEOLC Regular comms, trust board support, visible team available to offer support. Face to face learning #WeEOLC | |
|
@JeanetteMulher1
05 September 2017 20:09
|
@WeEOLC Hi all, proud to be an Oncology Ward Sister @nottmhospitals looking forward to hearing thoughts and ideas #WeEOLC | |
|
@NUHNursing
05 September 2017 20:09
|
@SarahFreer2 Excellent work @NUHCriticalCare #WeEoLC | |
|
@heblau
05 September 2017 20:10
|
Are you asking what people are already doing to support staff? Or what is needed? #WeEOLC | |
|
@JoyWharton1
05 September 2017 20:10
|
#WeEOLC Q1 Building relationships, coaching, giving feedback, helping, working with, modelling etc by Specialist Palliative Care team | |
|
@NUHNursing
05 September 2017 20:10
|
RT @daljitathwal: Important to start with what change do staff want to make #WeEOLC https://twitter.com/WeEOLC/status/905145328814391300 | |
|
@SarahFreer2
05 September 2017 20:10
|
#weEOLC working with staff priorities has been our focus https://twitter.com/WeEOLC/status/905145328814391300 | |
|
@StLukesPlymouth
05 September 2017 20:10
|
#WeEOLC hi from Plymouth. We have a team based in @Derriford_Hosp. 4,865 patient visits & 17 eol training forums for NHS last year. | |
|
@BridgetJohnst
05 September 2017 20:10
|
RT @heblau: Are you asking what people are already doing to support staff? Or what is needed? #WeEOLC | |
|
@WeEOLC
05 September 2017 20:10
|
great point from @daljitathwal what do others think? #WeEOLC https://twitter.com/daljitathwal/status/905145806222655490 | |
|
@SarahMullenEoLC
05 September 2017 20:10
|
Hi #WeEOLC End of Life Care Educator from @PennineAcuteNHS Striving to support the generalists to be the specialists #onechance | |
|
@PhilBallRN
05 September 2017 20:10
|
Helps to identify interested people first #WeEOLC they can show benefits to their peers, proactive reduction of anx… https://twitter.com/i/web/status/905146229700644864 | |
|
@BridgetJohnst
05 September 2017 20:11
|
Meaning? Interested to hear more #weeolc https://twitter.com/sarahfreer2/status/905146049630789633 | |
|
@ruth_pettit
05 September 2017 20:11
|
@WeEOLC @NUHCriticalCare #WeEOLC There are three separate units, each has a band 6 lead, supported by several band… https://twitter.com/i/web/status/905146337964032005 | |
|
@WeEOLC
05 September 2017 20:11
|
@suehaines1 @GeorginaKVL yes tell us more? #WeEOLC https://twitter.com/suehaines1/status/905145788774440961 | |
|
@WeEOLC
05 September 2017 20:11
|
RT @SarahFreer2: #weEOLC & we re v proud of what you ve achieved! https://twitter.com/ruth_pettit/status/905144916052934657 | |
|
@BridgetJohnst
05 September 2017 20:11
|
RT @WeEOLC: great point from @daljitathwal what do others think? #WeEOLC https://twitter.com/daljitathwal/status/905145806222655490 | |
|
@AgencyNurse
05 September 2017 20:12
|
RT @NUHEOLC: @WeEOLC @SarahFreer2 Empowering staff to take ownership of EOLC from the grass routes to trust board engagement #WeEOLC | |
|
@suehaines1
05 September 2017 20:12
|
sounds great Sarah, what education interventions have you found make the biggest difference? #weeolc https://twitter.com/SarahMullenEoLC/status/905146185542971393 | |
|
@JoyWharton1
05 September 2017 20:12
|
#WeEOLC Q1 sharing patient stories-especially when a Ward team achieves something special for a patient and family | |
|
@WeEOLC
05 September 2017 20:12
|
any tips or advice ? @SarahFreer2 @NUHEOLC @daljitathwal #WeEOLC https://twitter.com/NurseJoe87/status/905146325204951040 | |
|
@SarahFreer2
05 September 2017 20:12
|
#WeEolc we agree ownership by all vip https://twitter.com/fionaDmurphy/status/905146192962756609 | |
|
@WeEOLC
05 September 2017 20:13
|
RT @StLukesPlymouth: #WeEOLC 31% of all patients we care for are in @Derriford_Hosp, this is compared to only 7% in our traditional hosp… | |
|
@NUHNursing
05 September 2017 20:13
|
RT @ruth_pettit: @WeEOLC @NUHCriticalCare #WeEOLC There are three separate units, each has a band 6 lead, supported by several band… | |
|
@JoyWharton1
05 September 2017 20:14
|
#WeEOLC Q1 also using structured approaches such as Gold Standard Framework and Improvement methodologies | |
|
@KateMusson3
05 September 2017 20:14
|
Giving staff the confidence to have these conversations about EOLC. A communication session is included in my 3 day Oncology course #WeEOLC | |
|
@heblau
05 September 2017 20:14
|
Much depends on clinical context;what is needed in one acute area will not necessarily be so in another;sensitive & flexible support #WeEOLC | |
|
@danfurmedge
05 September 2017 20:14
|
Nurses understand it. And the bundle prompts them to ensure family are communicated with daily about progress. #weEOLC | |
|
@fionaDmurphy
05 September 2017 20:14
|
@SarahFreer2 Real time coaching, support as well as regular mandatory education for all is a must #WeEOLC @WeEOLC it works well | |
|
@NUHEOLC
05 September 2017 20:14
|
RT @daljitathwal: @JoyWharton1 Completely agree! Leadership at all levels - encourage & feedback #WeEOLC https://twitter.com/JoyWharton1/status/905146026079739910 | |
|
@WeEOLC
05 September 2017 20:15
|
yes! see https://www.ncbi.nlm.nih.gov/pubmed/26586686 #WeEOLC @danfurmedge https://twitter.com/danfurmedge/status/905146866991550464 | |
|
@jaqwhite1
05 September 2017 20:15
|
RT @StLukesPlymouth: #WeEOLC 31% of all patients we care for are in @Derriford_Hosp, this is compared to only 7% in our traditional hosp… | |
|
@SarahFreer2
05 September 2017 20:15
|
#weeolc rather than a blanket one way to do it, @NUHEOLC specialities have explored what would make a difference in… https://twitter.com/i/web/status/905147339781922818 | |
|
@PhilBallRN
05 September 2017 20:15
|
RT @StLukesPlymouth: #WeEOLC 31% of all patients we care for are in @Derriford_Hosp, this is compared to only 7% in our traditional hosp… | |
|
@suehaines1
05 September 2017 20:16
|
#WeEOLC so true and personalised family centred care at such a pivotal time families and carers will never forget https://twitter.com/GeorginaKVL/status/905147150727876608 | |
|
@WeEOLC
05 September 2017 20:16
|
RT @daljitathwal: Yep - staff at frontline know patient experience better than anyone else!! #WeEOLC https://twitter.com/WeEOLC/status/905146760129110017 | |
|
@SarahMullenEoLC
05 September 2017 20:16
|
RT @fionaDmurphy: Hello #WeEoLC every patient and family every time = everyone's business ?? | |
|
@WeEOLC
05 September 2017 20:16
|
RT @SarahFreer2: #weeolc rather than a blanket one way to do it, @NUHEOLC specialities have explored what would make a difference in… | |
|
@JoyWharton1
05 September 2017 20:16
|
#WeEOLC mixed experiences. Difficult to maintain with staff movement, workforce pressures, getting people released… https://twitter.com/i/web/status/905147747812200452 | |
|
@WeEOLC
05 September 2017 20:16
|
RT @fionaDmurphy: @SarahFreer2 Real time coaching, support as well as regular mandatory education for all is a must #WeEOLC @WeEOLC it work… | |
|
@suehaines1
05 September 2017 20:18
|
RT @SarahFreer2: #weeolc rather than a blanket one way to do it, @NUHEOLC specialities have explored what would make a difference in… | |
|
@AliDinning
05 September 2017 20:19
|
#WeEOLC I'm a Critical care outreach nurse and educator. Liaison between critical care teams and EOLC is crucial for many sick ward pts | |
|
@WeEOLC
05 September 2017 20:19
|
what do others think? #WeEOLC @hazeltonge https://twitter.com/hazeltonge/status/905147820801499136 | |
|
@NicolaFrame1
05 September 2017 20:20
|
@WeEOLC @SarahFreer2 @NUHEOLC staff should be encouraged to have EOLC plans in place early if possible #WeEOLC | |
|
@BridgetJohnst
05 September 2017 20:20
|
RT @WeEOLC: what do others think? #WeEOLC @hazeltonge https://twitter.com/hazeltonge/status/905147820801499136 | |
|
@WeEOLC
05 September 2017 20:21
|
#WeEOLC Q2: how can we show using a network of EOL champions improves quality? https://t.co/hYTQcMCcfc | |
|
@heblau
05 September 2017 20:21
|
@WeEOLC @SarahFreer2 @NUHEOLC Freudian slip. Unsung heroes #WeEOLC | |
|
@daljitathwal
05 September 2017 20:21
|
@fionaDmurphy SWAN is a great communication tool to engage ALL staff!! #WeEOLC https://twitter.com/fionaDmurphy/status/905147671526166528 | |
|
@WeEOLC
05 September 2017 20:22
|
don't forget to use #WeEOLC in all your tweets folks so we can see your words! | |
|
@NurseJoe87
05 September 2017 20:22
|
@WeEOLC @hazeltonge Still very much Medical led decision making - Should be MDT decision based on evidence #WeEOLC | |
|
@WeEOLC
05 September 2017 20:22
|
@heblau @SarahFreer2 @NUHEOLC i thought about leaving it as it was but....#WeEOLC :) | |
|
@WeEOLC
05 September 2017 20:22
|
RT @WeEOLC: #WeEOLC Q2: how can we show using a network of EOL champions improves quality? https://t.co/hYTQcMCcfc | |
|
@BridgetJohnst
05 September 2017 20:22
|
Although measuring quality of care is possible and important to evidence what we do #weeolc https://twitter.com/heblau/status/905148748111765504 | |
|
@NUHNursing
05 September 2017 20:22
|
RT @daljitathwal: @fionaDmurphy SWAN is a great communication tool to engage ALL staff!! #WeEOLC https://twitter.com/fionaDmurphy/status/905147671526166528 | |
|
@NUHNursing
05 September 2017 20:22
|
RT @WeEOLC: #WeEOLC Q2: how can we show using a network of EOL champions improves quality? https://t.co/hYTQcMCcfc | |
|
@WeEOLC
05 September 2017 20:23
|
@SarahMullenEoLC @SarahFreer2 @NUHEOLC hi sarah - don't forget #WeEOLC ! | |
|
@Nicki_Haywood
05 September 2017 20:23
|
RT @fionaDmurphy: Hello #WeEoLC every patient and family every time = everyone's business ?? | |
|
@NUHEOLC
05 September 2017 20:23
|
#WeEOLC https://twitter.com/nuheolc/status/905148730764079104 | |
|
@JoyWharton1
05 September 2017 20:23
|
#WeEOLC I've noticed that empowered staff on our wards source tea sets for family drinks, odd cups used in other ar… https://twitter.com/i/web/status/905149379446788101 | |
|
@SarahFreer2
05 September 2017 20:23
|
#weeolc we re using the CODE bereavement survey to help capture what we re doing & the feedbk allows us to focus th… https://twitter.com/i/web/status/905149383301267456 | |
|
@NUHEOLC
05 September 2017 20:23
|
RT @NUHEOLC: #WeEOLC https://twitter.com/nuheolc/status/905148730764079104 | |
|
@ShazzaHudson
05 September 2017 20:23
|
@WeEOLC Engagement and feedback. Work with bereaved families to improve service design. Use Voices. IPos maybe? #weeolc | |
|
@JeanetteMulher1
05 September 2017 20:23
|
@WeEOLC @hazeltonge Nurses are with patients 24/7 and often recognise the deterioration in patients and know them best #WeEOLC | |
|
@ShazzaHudson
05 September 2017 20:23
|
RT @WeEOLC: #WeEOLC Q2: how can we show using a network of EOL champions improves quality? https://t.co/hYTQcMCcfc | |
|
@daljitathwal
05 September 2017 20:23
|
Great question - for me its patient and carer feedback. I look at what complaints say - useful check! #WeEOLC https://twitter.com/WeEOLC/status/905148817699467264 | |
|
@WeEOLC
05 September 2017 20:24
|
@heblau @SarahFreer2 @NUHEOLC mesaure inouts, activities, outputs, outcomes (experice of ) #WeEOLC | |
|
@fionaDmurphy
05 September 2017 20:24
|
RT @SarahFreer2: #weeolc SWAN definately captures staffs hearts & minds https://twitter.com/fionaDmurphy/status/905147671526166528 | |
|
@heblau
05 September 2017 20:24
|
@BridgetJohnst Could think about approaches to evidence that recognise complexity eg action research #WeEOLC | |
|
@NUHNursing
05 September 2017 20:24
|
#WeEOLC definitely, clinical leadership https://twitter.com/nuheolc/status/905148730764079104 | |
|
@WeNurses
05 September 2017 20:24
|
Really interesting question #WeEOLC https://twitter.com/WeEOLC/status/905148817699467264 | |
|
@NUHNursing
05 September 2017 20:25
|
RT @WeEOLC: Q2d how can we show unsung a network of EOL champions improves EOLC @SarahFreer2 @NUHEOLC #WeEOLC https://t.co/GELY4CHKkN | |
|
@Nursey1982
05 September 2017 20:25
|
Using @schwartz_nuh rounding to help encourage open conversations around EOL care throughout the trust #WeEOLC https://twitter.com/weeolc/status/905148054965248000 | |
|
@WeEOLC
05 September 2017 20:25
|
RT @daljitathwal: Great question - for me its patient and carer feedback. I look at what complaints say - useful check! #WeEOLC https://t.c… | |
|
@NurseJoe87
05 September 2017 20:25
|
@daljitathwal Looking at doing 'In your shoes' events for relatives who have had hospital experiences - User feedback essential #WeEOLC | |
|
@ruth_pettit
05 September 2017 20:25
|
@WeEOLC Our EOLC champions get positive feedback from the bereavement meetings they hold with families. #WeEOLC | |
|
@BridgetJohnst
05 September 2017 20:25
|
Absolutely #weeolc collaborative approaches important here https://twitter.com/heblau/status/905149726533746690 | |
|
@WeEOLC
05 September 2017 20:26
|
this is amazing everyone - ill be posting stats and summary after tonight @SarahFreer2 #WeEOLC | |
|
@NUHEOLC
05 September 2017 20:26
|
By thinking of bereavement before death we can make a families journey that little bit smoother #WeEOLC #NUHEOLC | |
|
@suehaines1
05 September 2017 20:26
|
RT @Nursey1982: Using @schwartz_nuh rounding to help encourage open conversations around EOL care throughout the trust #WeEOLC https://t.co… | |
|
@daljitathwal
05 September 2017 20:26
|
@helenadurham Patients and Carers are the start and points!! #WeEOLC https://twitter.com/helenadurham/status/905148450567847937 | |
|
@BridgetJohnst
05 September 2017 20:26
|
RT @Nursey1982: Using @schwartz_nuh rounding to help encourage open conversations around EOL care throughout the trust #WeEOLC https://t.co… | |
|
@BridgetJohnst
05 September 2017 20:27
|
RT @NUHEOLC: By thinking of bereavement before death we can make a families journey that little bit smoother #WeEOLC #NUHEOLC | |
|
@NUHEOLC
05 September 2017 20:27
|
RT @WeEOLC: this is amazing everyone - ill be posting stats and summary after tonight @SarahFreer2 #WeEOLC | |
|
@jaqwhite1
05 September 2017 20:27
|
@JeanetteMulher1 @WeEOLC @hazeltonge And can help to recognise people at end of life if not already known #earlieridentification #WeEOLC | |
|
@WeEOLC
05 September 2017 20:27
|
Ok Q3: what are the challenges of engaging the full workforce in EOLC? #WeEOLC @SarahFreer2 @NUHEOLC https://t.co/R46Z5OcTOY | |
|
@NUHEOLC
05 September 2017 20:27
|
RT @ruth_pettit: @WeEOLC Our EOLC champions get positive feedback from the bereavement meetings they hold with families. #WeEOLC | |
|
@KarenLadybirdy
05 September 2017 20:27
|
RT @fionaDmurphy: Hello #WeEoLC every patient and family every time = everyone's business ?? | |
|
@BridgetJohnst
05 September 2017 20:29
|
RT @WeEOLC: @Nursey1982 @schwartz_nuh absolurely - anyone else using Schwartz rounds? #WeEOLC | |
|
@jaqwhite1
05 September 2017 20:29
|
RT @ruth_pettit: @WeEOLC Our EOLC champions get positive feedback from the bereavement meetings they hold with families. #WeEOLC | |
|
@WeEOLC
05 September 2017 20:29
|
#WeEOLC https://twitter.com/GeorginaKVL/status/905149373079851008 | |
|
@NurseJoe87
05 September 2017 20:29
|
@WeEOLC @SarahFreer2 @NUHEOLC Transient, large workforces and so many other changes happening. Lots for staff to take in #WeEOLC | |
|
@WeEOLC
05 September 2017 20:30
|
#WeEOLC https://twitter.com/GeorginaKVL/status/905149093181345793 | |
|
@WeEOLC
05 September 2017 20:30
|
RT @NurseJoe87: @WeEOLC @hazeltonge Still very much Medical led decision making - Should be MDT decision based on evidence #WeEOLC | |
|
@clairehenry_
05 September 2017 20:30
|
#WeEOLC as part of supporting improvement we have used an adapted 15 steps approach for eolc working with people with experience | |
|
@SarahFreer2
05 September 2017 20:30
|
#weeolc maintaining the profile against competing priorities an issue which is where the champions are key in keepi… https://twitter.com/i/web/status/905151227096428545 | |
|
@WeEOLC
05 September 2017 20:31
|
RT @SarahFreer2: #weeolc maintaining the profile against competing priorities an issue which is where the champions are key in keepi… | |
|
@jaqwhite1
05 September 2017 20:31
|
RT @SarahFreer2: #weeolc we re using the CODE bereavement survey to help capture what we re doing & the feedbk allows us to focus th… | |
|
@WeEOLC
05 September 2017 20:31
|
RT @SarahFreer2: #WeEOLC the key is staff thinking of bereavement before the death, focuses compassion @NUHEOLC https://twitter.com/ruth_pettit/status/905149996957401090 | |
|
@WeEOLC
05 September 2017 20:31
|
RT @SarahFreer2: #weeolc SWAN definately captures staffs hearts & minds https://twitter.com/fionaDmurphy/status/905147671526166528 | |
|
@SarahMullenEoLC
05 September 2017 20:31
|
RT @SarahFreer2: #weeolc maintaining the profile against competing priorities an issue which is where the champions are key in keepi… | |
|
@WeEOLC
05 September 2017 20:31
|
RT @SarahFreer2: #WeEolc we agree ownership by all vip https://twitter.com/fionaDmurphy/status/905146192962756609 | |
|
@WeEOLC
05 September 2017 20:33
|
whats your advice on that Sue? #WeEOLC @suechisholm01 https://twitter.com/suechisholm01/status/905151442369085440 | |
|
@heblau
05 September 2017 20:34
|
@SarahFreer2 @WeEOLC @NUHEOLC How could champions support staff to do this in real terms? And do they face obstacles? #WeEOLC | |
|
@janicemorg
05 September 2017 20:34
|
RT @Nursey1982: Using @schwartz_nuh rounding to help encourage open conversations around EOL care throughout the trust #WeEOLC https://t.co… | |
|
@WeEOLC
05 September 2017 20:35
|
@NurseJoe87 @SarahFreer2 @NUHEOLC how do you manage that? #WeEOLC | |
|
@GeorginaKVL
05 September 2017 20:35
|
@SarahFreer2 @NUHEOLC Yes! So so so true! This = planning and conversations earlier on #WeEOLC | |
|
@WeEOLC
05 September 2017 20:36
|
RT @suehaines1: Great idea #WeEOLC particularly as part of mulitprofessional induction https://twitter.com/ruth_pettit/status/905151674397974530 | |
|
@WeEOLC
05 September 2017 20:36
|
RT @ShazzaHudson: @marie7732 @IrishHospice I agree completely Marie. How can front line staff influence board level agreement? #WeEOLC | |
|
@JoyWharton1
05 September 2017 20:36
|
RT @hospicemanager: @WeEOLC @SarahFreer2 @NUHEOLC Helping workforce see the relevance, how they can play their part, #WeEOLC e.g. suppo… | |
|
@jaqwhite1
05 September 2017 20:37
|
@SarahFreer2 @WeEOLC Can also help to link impact of better EoLC with other priorities e.g. acute admissions, bed days etc. #WeEOLC | |
|
@AnnMarieRiley10
05 September 2017 20:37
|
RT @SarahFreer2: #WeEOLC the key is staff thinking of bereavement before the death, focuses compassion @NUHEOLC https://twitter.com/ruth_pettit/status/905149996957401090 | |
|
@WeEOLC
05 September 2017 20:37
|
Q4: so what are the developments in EOLC practice in your organisation? #WeEOLC please share!!! @SarahFreer2… https://twitter.com/i/web/status/905152960648314880 | |
|
@jaqwhite1
05 September 2017 20:37
|
RT @SarahFreer2: #WeEOLC the key is staff thinking of bereavement before the death, focuses compassion @NUHEOLC https://twitter.com/ruth_pettit/status/905149996957401090 | |
|
@PhilBallRN
05 September 2017 20:37
|
@ShazzaHudson @marie7732 @IrishHospice We've begun clinical storytelling at beginning of Board meetings, #WeEolc gi… https://twitter.com/i/web/status/905152993317842946 | |
|
@WeEOLC
05 September 2017 20:38
|
RT @GeorginaKVL: @SarahFreer2 @NUHEOLC Yes! So so so true! This = planning and conversations earlier on #WeEOLC | |
|
@WeEOLC
05 September 2017 20:38
|
RT @WeEOLC: @NurseJoe87 @SarahFreer2 @NUHEOLC how do you manage that? #WeEOLC | |
|
@ShazzaHudson
05 September 2017 20:38
|
@DeeDavies12 @WeEOLC @SarahFreer2 @NUHEOLC I really liked this example of @DeathCafe with Doctors https://youtu.be/4mgS2dBduWA #WeEOLC | |
|
@WeEOLC
05 September 2017 20:38
|
RT @WeEOLC: @NUHNursing @NUHEOLC where can we find out more? #WeEOLC | |
|
@suehaines1
05 September 2017 20:39
|
RT @WeEOLC: Q4: so what are the developments in EOLC practice in your organisation? #WeEOLC please share!!! @SarahFreer2… | |
|
@StLukes_AtHome6
05 September 2017 20:39
|
RT @StLukesPlymouth: #WeEOLC 31% of all patients we care for are in @Derriford_Hosp, this is compared to only 7% in our traditional hosp… | |
|
@NUHEOLC
05 September 2017 20:40
|
RT @clairehenry_: #WeEOLC as part of supporting improvement we have used an adapted 15 steps approach for eolc working with people with… | |
|
@heblau
05 September 2017 20:40
|
@SarahFreer2 @WeEOLC Yes, the little things. And there's evidence ... https://www.kingsfund.org.uk/blog/2011/01/improving-patient-experience-its-little-things-matter #WeEOLC | |
|
@LearnPEOLC
05 September 2017 20:40
|
@hospicemanager @ShazzaHudson @marie7732 @IrishHospice That sounds amazing! Where can we find out more? #WeEOLC | |
|
@LearnPEOLC
05 September 2017 20:40
|
RT @WeEOLC: Q4: so what are the developments in EOLC practice in your organisation? #WeEOLC please share!!! @SarahFreer2… | |
|
@LearnPEOLC
05 September 2017 20:40
|
RT @WeEOLC: @NurseJoe87 @SarahFreer2 @NUHEOLC how do you manage that? #WeEOLC | |
|
@LearnPEOLC
05 September 2017 20:40
|
RT @SarahFreer2: #WeEOLC reassuring staff that small actions are so significant, families & pts remember | |
|
@mootootroo
05 September 2017 20:41
|
@WeEOLC #weEOLC q3 challenge = others don't always see as their role when it's everyone's responsibility | |
|
@WeEOLC
05 September 2017 20:41
|
RT @SarahFreer2: #WeEOLC reassuring staff that small actions are so significant, families & pts remember | |
|
@WeEOLC
05 September 2017 20:42
|
RT @mootootroo: @WeEOLC #weEOLC q3 challenge = others don't always see as their role when it's everyone's responsibility | |
|
@BridgetJohnst
05 September 2017 20:42
|
@marie7732 @IrishHospice It's great work Marie #weeolc | |
|
@jaqwhite1
05 September 2017 20:42
|
RT @JoyWharton1: #WeEOLC agree, we also 'sneak' training into training on other topics, e.g. Provide death cafes on development days https:… | |
|
@WeEOLC
05 September 2017 20:42
|
@marie7732 thank you for the link really important #WeEOLC | |
|
@IrishHospice
05 September 2017 20:42
|
Bereaved relatives surveyed in Ireland say single room made a real difference 2 care they & patient rcvd http://www.mater.ie/services/end-of-life-care/Survey-of-bereaved-family-members.pdf #WeEOLC | |
|
@WeEOLC
05 September 2017 20:43
|
a quick shout out to #pallcareweek and @AIIHPC - do follow their threads this week #weeolc | |
|
@jaqwhite1
05 September 2017 20:43
|
RT @SarahFreer2: #WeEOLC reassuring staff that small actions are so significant, families & pts remember | |
|
@WeEOLC
05 September 2017 20:43
|
RT @JoyWharton1: @ShazzaHudson @DeeDavies12 @WeEOLC @SarahFreer2 @NUHEOLC @DeathCafe @IanDewar @UHMBT #WeEOLC We use death cafes to… | |
|
@PhilBallRN
05 September 2017 20:44
|
RT @JoyWharton1: @ShazzaHudson @DeeDavies12 @WeEOLC @SarahFreer2 @NUHEOLC @DeathCafe @IanDewar @UHMBT #WeEOLC We use death cafes to… | |
|
@fionaDmurphy
05 September 2017 20:44
|
RT @WeEOLC: a quick shout out to #pallcareweek and @AIIHPC - do follow their threads this week #weeolc | |
|
@NUHNursing
05 September 2017 20:44
|
@WeEOLC @NUHEOLC I'm sure @SarahFreer2 will share our tool if DM her #weeolc | |
|
@PhilBallRN
05 September 2017 20:44
|
RT @WeEOLC: a quick shout out to #pallcareweek and @AIIHPC - do follow their threads this week #weeolc | |
|
@ShazzaHudson
05 September 2017 20:44
|
@GeorginaKVL @WeEOLC @SarahFreer2 @NUHEOLC Maintaining Presence is a wonderful phrase, #WeEOLC | |
|
@JeanetteMulher1
05 September 2017 20:44
|
@marie7732 @WeEOLC Agree, so important, awful if no sideroom available when privacy for families is so important #WeEOLC | |
|
@WeEOLC
05 September 2017 20:44
|
@SarahFreer2 @NUHEOLC we are getting some amazing sharing of developments you are all doing- please keep sharing #WeEOLC | |
|
@WeEOLC
05 September 2017 20:45
|
@GeorginaKVL @SarahFreer2 @NUHEOLC thats reallly intersting - we cant wait to read it! please add #WeEOLC to your t… https://twitter.com/i/web/status/905154971330650112 | |
|
@NurseJoe87
05 September 2017 20:45
|
Also working with @HWStaffordshire to arrange interviews about EOL experiences in hospital #WeEOLC | |
|
@WeEOLC
05 September 2017 20:45
|
RT @NUHNursing: @WeEOLC @NUHEOLC I'm sure @SarahFreer2 will share our tool if DM her #weeolc | |
|
@AnnMarieRiley10
05 September 2017 20:46
|
@GeorginaKVL @WeEOLC @SarahFreer2 @NUHEOLC So agree with this #WeEOLC | |
|
@WeEOLC
05 September 2017 20:46
|
fabulos thank you #WeEOLC https://twitter.com/Nursey1982/status/905154802186846210 | |
|
@NurseJoe87
05 September 2017 20:46
|
And using @hwb999 Homeward Bound and @SAGEandTHYME_ Comms skills training #WeEOLC | |
|
@WeEOLC
05 September 2017 20:46
|
RT @ShazzaHudson: @GeorginaKVL @WeEOLC @SarahFreer2 @NUHEOLC Maintaining Presence is a wonderful phrase, #WeEOLC | |
|
@WeEOLC
05 September 2017 20:46
|
@ShazzaHudson @GeorginaKVL @SarahFreer2 @NUHEOLC i think its brilliant #WeEOLC | |
|
@heblau
05 September 2017 20:46
|
Agree; being not doing. Busyness can get in the way of doing the right thing #WeEOLC | |
|
@WeEOLC
05 September 2017 20:48
|
RT @NurseJoe87: Also working with @HWStaffordshire to arrange interviews about EOL experiences in hospital #WeEOLC | |
|
@AnnMarieRiley10
05 September 2017 20:48
|
RT @helenadurham: @WeEOLC #WeEOLC This is really worth a listen http://www.bbc.co.uk/programmes/b092sp37 Need to get everyone talking about dying - it's com… | |
|
@100anne
05 September 2017 20:48
|
@WeEOLC @AIIHPC Yes they have been interesting #WeEolc | |
|
@AgencyNurse
05 September 2017 20:49
|
RT @helenadurham: @WeEOLC #WeEOLC This is really worth a listen http://www.bbc.co.uk/programmes/b092sp37 Need to get everyone talking about dying - it's com… | |
|
@WeNurses
05 September 2017 20:49
|
RT @helenadurham: @WeEOLC #WeEOLC This is really worth a listen http://www.bbc.co.uk/programmes/b092sp37 Need to get everyone talking about dying - it's com… | |
|
@BridgetJohnst
05 September 2017 20:49
|
Good point - Benner one of first nurses to talk about 'presencing' 1984 novice to expert #weeolc https://twitter.com/georginakvl/status/905153557262950400 | |
|
@fionaDmurphy
05 September 2017 20:49
|
RT @helenadurham: @WeEOLC #WeEOLC This is really worth a listen http://www.bbc.co.uk/programmes/b092sp37 Need to get everyone talking about dying - it's com… | |
|
@heblau
05 September 2017 20:49
|
@helenadurham @WeEOLC Yes, think @mgtmccartney talks a LOT of sense! #WeEOLC | |
|
@WeNurses
05 September 2017 20:49
|
RT @WeEOLC: Q4: so what are the developments in EOLC practice in your organisation? #WeEOLC please share!!! @SarahFreer2… | |
|
@clairehenry_
05 September 2017 20:49
|
RT @helenadurham: @WeEOLC #WeEOLC This is really worth a listen http://www.bbc.co.uk/programmes/b092sp37 Need to get everyone talking about dying - it's com… | |
|
@NurseJoe87
05 September 2017 20:49
|
@WeEOLC West Miss Specialist Palliative Care Prescribing Forum coming soon too! #WeEOLC | |
|
@daljitathwal
05 September 2017 20:50
|
RT @helenadurham: @WeEOLC #WeEOLC This is really worth a listen http://www.bbc.co.uk/programmes/b092sp37 Need to get everyone talking about dying - it's com… | |
|
@NUHNursing
05 September 2017 20:50
|
@Nursey1982 @teamEDnuh @LorraineHourd @Tracykeane7 @NewtonJane8 such excellent work being led in ED #WeEOLC | |
|
@LearnPEOLC
05 September 2017 20:51
|
RT @BridgetJohnst: Our @EndofLifeStudy group looking at this #weeolc https://twitter.com/alresfordbear/status/905155462563340289 | |
|
@LearnPEOLC
05 September 2017 20:51
|
RT @AlresfordBear: Indeed. So its my choice. #WeEOLC https://twitter.com/helenadurham/status/905155669459918848 | |
|
@LearnPEOLC
05 September 2017 20:51
|
RT @WeEOLC: Q5: ok....from tonight or in general from this topic- what are YOU going to put into practice? #WeEOLC @SarahFreer2… | |
|
@LearnPEOLC
05 September 2017 20:51
|
RT @NUHNursing: @Nursey1982 @teamEDnuh @LorraineHourd @Tracykeane7 @NewtonJane8 such excellent work being led in ED #WeEOLC | |
|
@LearnPEOLC
05 September 2017 20:51
|
RT @NurseJoe87: @WeEOLC West Miss Specialist Palliative Care Prescribing Forum coming soon too! #WeEOLC | |
|
@LearnPEOLC
05 September 2017 20:51
|
RT @heblau: @helenadurham @WeEOLC Yes, think @mgtmccartney talks a LOT of sense! #WeEOLC | |
|
@NUHNursing
05 September 2017 20:51
|
RT @WeEOLC: Q5: ok....from tonight or in general from this topic- what are YOU going to put into practice? #WeEOLC @SarahFreer2… | |
|
@LearnPEOLC
05 September 2017 20:51
|
RT @BridgetJohnst: Good point - Benner one of first nurses to talk about 'presencing' 1984 novice to expert #weeolc https://twitter.com/georginakvl/status/905153557262950400 | |
|
@LearnPEOLC
05 September 2017 20:52
|
RT @100anne: @WeEOLC @AIIHPC Yes they have been interesting #WeEolc | |
|
@LearnPEOLC
05 September 2017 20:52
|
RT @helenadurham: @WeEOLC #WeEOLC This is really worth a listen http://www.bbc.co.uk/programmes/b092sp37 Need to get everyone talking about dying - it's com… | |
|
@LearnPEOLC
05 September 2017 20:52
|
RT @heblau: @AlresfordBear have collected some data but not got around to analysing yet ... #WeEOLC | |
|
@NUHEOLC
05 September 2017 20:52
|
RT @ruth_pettit: @WeEOLC @SarahFreer2 @NUHEOLC #WeEOLC partnership working with HPCT, chaplaincy, SNOD, lead medical consultant and… | |
|
@LearnPEOLC
05 September 2017 20:52
|
RT @JoyWharton1: #WeEOLC we join together across the locality to provide study days for staff from acute, community and care homes t… | |
|
@stowe_emily
05 September 2017 20:52
|
@JoyWharton1 We do similar - offering joint training across hospice, community and acute services #WeEOLC | |
|
@NUHNursing
05 September 2017 20:52
|
RT @helenadurham: @WeEOLC #WeEOLC This is really worth a listen http://www.bbc.co.uk/programmes/b092sp37 Need to get everyone talking about dying - it's com… | |
|
@SarahFreer2
05 September 2017 20:52
|
#weeolc we re looking at engaging medical staff, this could be a useful option @NUHEOLC https://twitter.com/AlresfordBear/status/905155462563340289 | |
|
@jaqwhite1
05 September 2017 20:53
|
@helenadurham @clairehenry_ @WeEOLC Completely agree - #nevertooearly #WeEOLC | |
|
@WeEOLC
05 September 2017 20:53
|
RT @JoyWharton1: We support Board rounds (quick MDTs) in AMU to identify patients who would benefit from a palliative approach #WeEOLC | |
|
@SarahFreer2
05 September 2017 20:53
|
#weeolc looking at how we engage with tissue donation conversations early on https://twitter.com/ruth_pettit/status/905156435792842756 | |
|
@NurseJoe87
05 September 2017 20:53
|
RT @JoyWharton1: We support Board rounds (quick MDTs) in AMU to identify patients who would benefit from a palliative approach #WeEOLC | |
|
@NUHEOLC
05 September 2017 20:53
|
RT @JoyWharton1: We support Board rounds (quick MDTs) in AMU to identify patients who would benefit from a palliative approach #WeEOLC | |
|
@NUHEOLC
05 September 2017 20:54
|
RT @NurseJoe87: @WeEOLC West Miss Specialist Palliative Care Prescribing Forum coming soon too! #WeEOLC | |
|
@AnnMarieRiley10
05 September 2017 20:54
|
RT @LesleyReilly20: @WeEOLC @SarahFreer2 @NUHEOLC #weEOLC @sarahfreer2 actions speak loader than words it's in all our gift to enthuse eng… | |
|
@WeEOLC
05 September 2017 20:54
|
RT @SarahFreer2: #weeolc looking at how we engage with tissue donation conversations early on https://t.co/6zEHBCwuTe | |
|
@DeeDavies12
05 September 2017 20:54
|
@WeEOLC @SarahFreer2 @NUHEOLC Sharing EDOP patient/person story at Trust Board #WeEOLC | |
|
@WeEOLC
05 September 2017 20:54
|
RT @LesleyReilly20: @WeEOLC @SarahFreer2 @NUHEOLC #weEOLC @sarahfreer2 actions speak loader than words it's in all our gift to enthuse eng… | |
|
@NUHEOLC
05 September 2017 20:54
|
RT @SarahFreer2: #weeolc we re looking at engaging medical staff, this could be a useful option @NUHEOLC https://t.co/myHuxLVGHl | |
|
@AliDinning
05 September 2017 20:54
|
RT @stowe_emily: @JoyWharton1 We do similar - offering joint training across hospice, community and acute services #WeEOLC | |
|
@JoyWharton1
05 September 2017 20:54
|
@heblau @GeorginaKVL @WeEOLC @SarahFreer2 @NUHEOLC #WeEOLC staff need to proactively offer, not wait to be asked about open visiting. | |
|
@PhilBallRN
05 September 2017 20:55
|
@WeEOLC @SarahFreer2 @NUHEOLC Review links with local hospital teams #WeEolc work harder at relationships to suppor… https://t.co/R3VkNpIxH2 | |
|
@WeEOLC
05 September 2017 20:55
|
Last 5 minutes!! #WeEOLC what are you going to put into practice? https://t.co/IeZDc8aemk | |
|
@GeorginaKVL
05 September 2017 20:55
|
@AlresfordBear Very true. But together (wider society together) we can overcome some of those obstacles #weEOLC | |
|
@SarahFreer2
05 September 2017 20:55
|
RT @JoyWharton1: @heblau @GeorginaKVL @WeEOLC @SarahFreer2 @NUHEOLC #WeEOLC staff need to proactively offer, not wait to be asked about ope… | |
|
@LearnPEOLC
05 September 2017 20:55
|
RT @SarahFreer2: #weeolc looking at how we engage with tissue donation conversations early on https://twitter.com/ruth_pettit/status/905156435792842756 | |
|
@NUHEOLC
05 September 2017 20:55
|
RT @SarahFreer2: #weeolc looking at how we engage with tissue donation conversations early on https://twitter.com/ruth_pettit/status/905156435792842756 | |
|
@LearnPEOLC
05 September 2017 20:55
|
RT @hospicemanager: @WeEOLC @SarahFreer2 @NUHEOLC Review links with local hospital teams #WeEolc work harder at relationships to suppor… | |
|
@AgencyNurse
05 September 2017 20:55
|
RT @WeEOLC: Last 5 minutes!! #WeEOLC what are you going to put into practice? https://t.co/IeZDc8aemk | |
|
@AnnMarieRiley10
05 September 2017 20:55
|
RT @JoyWharton1: @heblau @GeorginaKVL @WeEOLC @SarahFreer2 @NUHEOLC #WeEOLC staff need to proactively offer, not wait to be asked about ope… | |
|
@suechisholm01
05 September 2017 20:56
|
@WeEOLC @SarahFreer2 @NUHEOLC I'm hoping to be more enabling in every interaction with colleagues, open dialogue, actively encourage #weEOLC | |
|
@clairehenry_
05 September 2017 20:56
|
RT @DeeDavies12: @WeEOLC @SarahFreer2 @NUHEOLC Sharing EDOP patient/person story at Trust Board #WeEOLC | |
|
@jaqwhite1
05 September 2017 20:56
|
RT @JoyWharton1: We support Board rounds (quick MDTs) in AMU to identify patients who would benefit from a palliative approach #WeEOLC | |
|
@LearnPEOLC
05 September 2017 20:56
|
I'm going to look at this thread in detail as so much info and resources #WeEOLC https://twitter.com/weeolc/status/905157472532537347 | |
|
@NurseJoe87
05 September 2017 20:56
|
Joint training with our local hospices @DougieMacStoke to share best practice #WeEOLC | |
|
@NUHEOLC
05 September 2017 20:56
|
RT @JoyWharton1: @heblau @GeorginaKVL @WeEOLC @SarahFreer2 @NUHEOLC #WeEOLC staff need to proactively offer, not wait to be asked about ope… | |
|
@danfurmedge
05 September 2017 20:56
|
@NUHEOLC You need to ask @drlaurajane about that #WeEOLC | |
|
@daljitathwal
05 September 2017 20:57
|
Great to be involved in @NHSImprovement EOLC collaboratives, enabling Trusts to do fab work @mrsjmckenna @SherreeFagge #WeEoLC | |
|
@NUHNursing
05 September 2017 20:57
|
@heblau @GeorginaKVL @WeEOLC @SarahFreer2 @NUHEOLC Sad to hear open visiting end of life care is not normal practice! #weeolc | |
|
@heblau
05 September 2017 20:57
|
@danfurmedge @NUHEOLC @drlaurajane Have a peep at this http://deathcafe.com/ #WeEOLC | |
|
@jaqwhite1
05 September 2017 20:57
|
@heblau @helenadurham @clairehenry_ @WeEOLC Yes, how can we change that? #WeEOLC | |
|
@cookefamily5
05 September 2017 20:58
|
RT @fionaDmurphy: Hello #WeEoLC every patient and family every time = everyone's business ?? | |
|
@AgencyNurse
05 September 2017 20:58
|
Thank you #WeEOLC - been mostly lurking but some great stuff to think on | |
|
@PhilBallRN
05 September 2017 20:58
|
RT @learnhospice: I'm going to look at this thread in detail as so much info and resources #WeEOLC https://twitter.com/weeolc/status/905157472532537347 | |
|
@WeEOLC
05 September 2017 20:58
|
RT @GeorginaKVL: @AlresfordBear Very true. But together (wider society together) we can overcome some of those obstacles #weEOLC | |
|
@WeEOLC
05 September 2017 20:58
|
RT @WeEOLC: Last 5 minutes!! #WeEOLC what are you going to put into practice? https://t.co/IeZDc8aemk | |
|
@WeEOLC
05 September 2017 20:58
|
RT @hospicemanager: @WeEOLC @SarahFreer2 @NUHEOLC Review links with local hospital teams #WeEolc work harder at relationships to suppor… | |
|
@WeEOLC
05 September 2017 20:58
|
RT @JoyWharton1: @heblau @GeorginaKVL @WeEOLC @SarahFreer2 @NUHEOLC #WeEOLC staff need to proactively offer, not wait to be asked about ope… | |
|
@WeEOLC
05 September 2017 20:58
|
RT @DeeDavies12: @WeEOLC @SarahFreer2 @NUHEOLC Sharing EDOP patient/person story at Trust Board #WeEOLC | |
|
@NUHNursing
05 September 2017 20:59
|
RT @LesleyReilly20: @WeEOLC @SarahFreer2 @NUHEOLC #weEOLC @sarahfreer2 actions speak loader than words it's in all our gift to enthuse eng… | |
|
@SarahFreer2
05 September 2017 20:59
|
#weeolc need to support medical colleagues to be brave & honest https://t.co/QQsuJfY1pZ | |
|
@PhilBallRN
05 September 2017 20:59
|
RT @AgencyNurse: Thank you #WeEOLC - been mostly lurking but some great stuff to think on | |
|
@WeEOLC
05 September 2017 20:59
|
#WeEOLC https://t.co/3GntVX233R | |
|
@BridgetJohnst
05 September 2017 20:59
|
RT @ruth_pettit: @WeEOLC @SarahFreer2 @NUHEOLC #WeEOLC also currently planning a memorial service for @NUHCriticalCare relatives for 2018.… | |
|
@WeEOLC
05 September 2017 20:59
|
RT @learnhospice: I'm going to look at this thread in detail as so much info and resources #WeEOLC https://t.co/gdrKKh3gRr | |
|
@AlresfordBear
05 September 2017 20:59
|
@GeorginaKVL Not sure. Would like to think so, what is wider society and when will it arrive to tackle social inequity? #WeEOLC | |
|
@LesleyReilly20
05 September 2017 20:59
|
@WeEOLC @sarahfreer2 #WeEOLC thank you for the opportunity for such an important discussion @weEOLC |



